When Sleep Evades You, Cognitive Behavioural Therapy Might Help

A third of Canadians report getting less than the recommended minimum of seven hours of sleep a night, while 15 per cent meet the criteria for insomnia. Experts say the frontline treatment is cognitive behavioural therapy. Photo: Alessandro De Carli/EyeEm
Do you get enough sleep? Do you sleep well?
These are important questions when you consider that insufficient sleep — defined as short duration and/or poor quality — is associated with health outcomes including obesity, Type 2 diabetes, cardiovascular disease, depression, irritability, and a reduction in general well-being.
According to a 2017 report from Statistics Canada, for many of us, the answers are no and no.
- A third of Canadians reported getting less than the recommended minimum of seven hours of sleep a night.
- About half of Canadians (55 per cent of women and 43 per cent of men) answered “sometimes/most of the time/all of the time” when asked whether they have trouble falling or staying asleep.
And when the statisticians looked deeper into the data for a follow-up report last year, they found that as many as 15 per cent of us meet the criteria for insomnia. That is, we’re dissatisfied with our sleep and feel like it’s impacting our daytime functioning.
And although there’s an ever-growing assortment of products promising to improve sleep — everything from aromatherapy to weighted blankets — for insomniacs, it may be time to consider therapy.
“This is the thing with insomnia. It often doesn’t just resolve on its own and actually requires treatment,” says Katherine Rasmussen, director of behavioural sleep medicine at the Centre for Sleep & Human Performance in Calgary.
Cognitive behavioural therapy for insomnia (CBT-I) has been shown to work so well that it’s the recommended first-line treatment in Canada.
“It’s about 70 to 80 per cent effective,” Rasmussen says. “And we also use it to help people taper off their sleep medication.”
As she explains, CBT-I helps patients change maladaptive behaviours, one of which is spending too much time in bed.
“They become desperate for more sleep, and one of the strategies they use is going to bed earlier and staying in bed later. But this actually worsens the sleep. It fragments it even further because they don’t have enough sleep pressure.”
Can Sleep Apps Help?
Relaxation training, another pillar of CBT-I, also helps, and it can include using popular meditation apps like Calm and Headspace, Rasmussen says.
“People just can’t turn off the brain. And so anything to help bring down that hyper-arousal is very important. And that’s a great example of using technology positively to help us relax.”
CBT-I can take as little as just over a month and the effects can be long-lasting, says Toronto-based psychologist Dr. Khush Amaria.
“You’re in treatment — active therapy, let’s say – for about six weeks or so. And statistically, we see effects that continue for another year or two,” she says. “I say a year or two because we often don’t examine people after that. So it’s possible that sleep is fine for longer.”
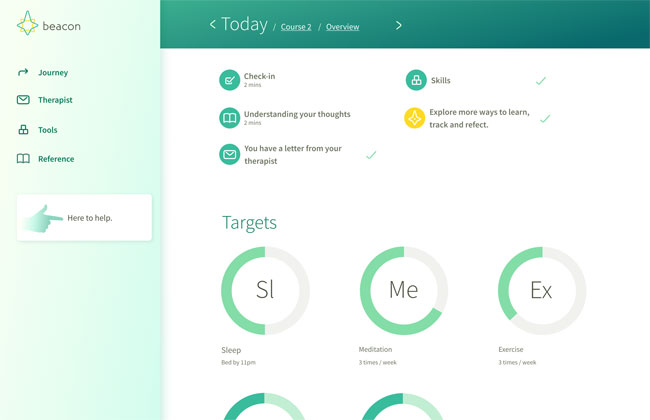
Amaria is an expert in cognitive behavioural therapy and the senior clinical director for Beacon, a clinician-guided digital therapy service that recently added CBT-I to its program.
Users start with a detailed online assessment and then move on to daily tracking and therapist-directed behavioural changes. That could include adjusting bedtime, exercising more often and avoiding daily naps. (Yes, that snooze on the couch every afternoon could be interfering with nightly sleep.)
Beyond lifestyle habits, mental health factors can also contribute to insomnia and would be addressed in a user’s treatment plan.
“There are higher rates of what we call comorbidity. So they meet criteria for both insomnia and mental health issues, with depression and anxiety being the most common of those,” Amaria explains.
Beacon’s digital therapy options start at $595, and the service is covered by most benefits plans in Canada.
Albertans are lucky, Rasmussen points out, that sleep therapy programs are provincially funded but says online services, like that of Beacon’s, provide an opportunity for people who may not have access to CBT-I in their community or for whom it’s cost-prohibitive to see a psychologist.
“They’re structured programs, which are not as individualized as working with a therapist, but they cover many good, relevant aspects of sleep that I think have good value for patients.”
Do You Have Insomnia?
The Canadian Sleep Society (CSS) defines insomnia as “difficulty sleeping at least three nights a week for at least one month and that is associated with impaired functioning or distress.”
Risk Factors for Insomnia
According to the CSS, the following factors can increase risk of insomnia: increasing age, being female, an anxiety-prone personality, family history of insomnia and having medical and mental illnesses. Major life events such as marital separation or illness can precipitate the onset of insomnia.
RELATED:
Fitness, Sleep and Everything In-Between: 8 Must-Have Apps You Can Download For Free
How Melatonin and Better Sleep Habits Can Help You Live Longer